Cauterization - Cancer Team, Division of Gastroenterology and Hepatology, Taipei Tzu Chi Hospital
By: Wang Chia-Chi, Director of Division of Gastroenterology and Hepatology, Taipei Tzu Chi Hospital
Liver is a silent organ.
In the past three decades, convenient lifestyle and prevalent hepatitis B,
liver cancer, a disease difficult to treat, has always been ranked first or
second in the Top Ten Cancer among Taiwanese.
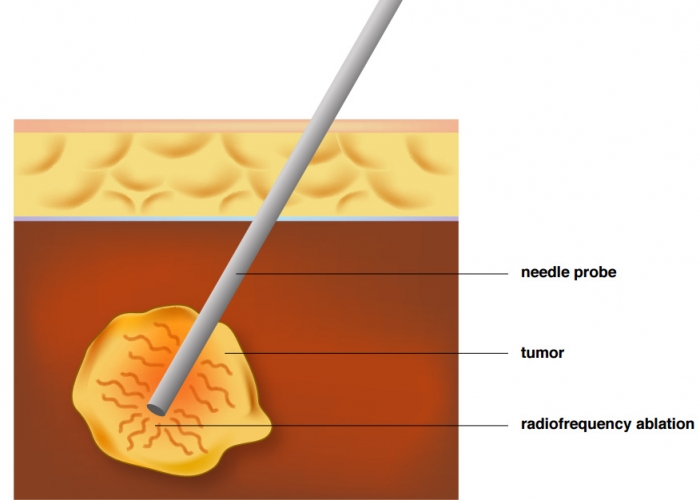
Radiofrequency ablation is, in other words,
is to cauterize liver tumor with heat via a tiny needle,
which can successfully shrink and remove cancer cells without entering
the operation room.
It is a empathetic therapy from the Division of Gastroenterology and
Hepatology of Taipei Tzu Chi Hospital to our patients.
RFA cauterize the tumor with a needle to evaporate and ablate the cancer cells
Mr. Li, 47 years old, was hospitalized several years ago due to black stool and hematemesis. He thought he was healthy, only to discover upon further examinations that he was suffering from hepatitis B, poor liver function, signs of cirrhosis and multiple tumors. The physicians of Gastroenterology and Hepatology first utilized embolism to reduce the tumor size and administered antiviral drugs to stop liver inflammation and improve liver function. The condition seemed to brighten up, but a tumor with a diameter of 4.5cm never shrank during the entire treatment, and had to be dealt with other treatments.
Tumor Ablation through Needle Cauterization
Tumor of such significant size are usually removed surgically, but the risk of surgery was too high for Mr. Li with his poor liver function, therefore needle cauterization was recommended. Usual needles, though, can only cauterize tumors smaller than 3cm in diameter, and this tumor was already 4.5cm, which demanded two needles or more to successfully remove the tumor. The application of this cauterization would require the guidance of ultrasound to pinpoint the tumor location, cauterize the tumor with both needles to ablate the tumor without damaging nearby tissues. Something unique about Mr. Li’s case was that the tumor located above where bile duct branches out and below the large intestines, if the needle went too deep and damaged the bile duct it would cause jaundice, too shallow would risk cauterizing the large intestines. In addition to accurate probing and positioning, another layer of protection must be applied, and that is artificial ascites.
The method was to inject large quantity of physiological saline into the patient’s abdomen to create a “moat” between the large intestines and the liver tumor. By doing so, the chance of perforation on the large intestines due to high heat would be minimized. Furthermore, the patient’s tumor was located near liver surface, where nerves are present, and the patient would experience severe pain if not anesthetized. In Taipei Tzu Chi Hospital, there are anesthetist routinely stationed at the examination room of Gastroenterology and Hepatology ward, and they can service the patient on-site, without moving the patient into the operating room, on demand. They allow the patient to take a long and relaxing slumber and wake up after the treatment is completed. Mr. Li underwent two two-needle treatments, and a month later, the CT images indicated no sign of tumor. He is still currently under outpatient follow-up.
Mr. Chu, worked in the market, was 47 years old as well. He was a drinker. Although he did not have hepatitis B or C, two years ago he, because to abnormal liver function, went to Taipei Tzu Chi Hospital for examination, and the result was alcoholic cirrhosis. He had to, in addition to regular outpatient visits, quit alcohol once and for all. During a routine check up, the abdominal ultrasound revealed a 2cm tumor, located below the right hepatic diaphragm, and a follow up CT scan identified it as malignant. As Mr. Chu concerned about the upcoming treatment, he saw, accidentally, the T.V. show “Tzu Chi Doctors” on Daai T.V., introducing liver tumor cauterization with artificial ascites, and he visited the hospital to understand the treatment and its effectiveness. The success rate of cauterizing a 2cm tumor is fairly high, but since Mr. Chu’s tumor was located at the right anterior lobe of the liver, close to the diaphragm and lungs, which made insertion difficult; furthermore, the chance of damaging the lung during treatment, leading to pneumothorax or hemothorax, is fairly high. With a successful injection of artificial ascites, not only would the tumor be more visible under ultrasound, the lung could be protected from any damage. Mr. Chu decided to accept this treatment. After hospitalization, 1,500cc of physiological saline was injected into the patient’s abdomen, and a successful cauterization treatment ensued. The CT scan a month after the operation indicated that the liver cancer had been removed, and Mr. Chu is still under outpatient follow up.
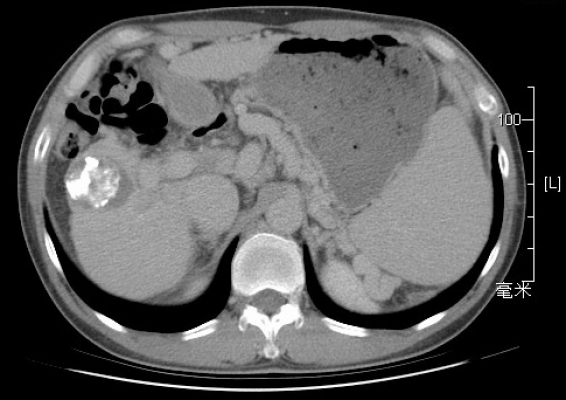
photo1: Prior to treatment, the patient, after a CT scan, is diagnosed with a large liver tumor.
photo2: After RFA treatment, CT scan during the follow-up one month later indicated the tumor had been cauterized and ablated. The white shadow on the tumor is the marks of prior embolization.
Hepatitis is a national disease. Taiwan’s leading cause of death is cancer, while liver cancer is ranked second in the incidence of cancer, behind only colorectal cancer. The criticality of liver cancer treatment lies in early diagnosis, therefore regular follow up of high-risk patients, such as those suffering from hepatitis B and C, cirrhosis or has a family history of liver cancer, is vital. Once liver cancer is present, it the impact would be severe to both the patient and the patient’s families. Doctors and patients usually share the same hope: to cure liver cancer. Curative treatments currently include surgery, or regional treatment such as radiofrequency ablation and liver transplant. Surgical treatment is often the top priority, but large wounds, high risk and long recovery are the down sides, while those with poor liver or cardiopulmonary functions, operation is not an option. Liver transplant is the last line of defense in terms of curative treatment, yet livers are hard to come by in Taiwan, and long term use of antirejection drugs are required even with a successful operation. Radiofrequency ablation, however, provided a treatment with low risk, small wound and speedy recovery. According to current research, the survival rate of radiofrequency ablation is similar to that of surgery.
Radiofrequency ablation primarily use a needle to cauterize tumors. One end of the needle is attached to the machine, and through the guidance of ultrasound imaging, insert the needle in vitro into the liver tumor. The machine would then introduce current into the needle and generate heat through high frequency alternating current, which would evaporate and eventually ablate the cancer cells by raising its temperature. The cauterizing region is oval shaped. To avoid carbonization due to needle overheating, which would reduce the sphere of cauterization, cold water is circulated through the needle.
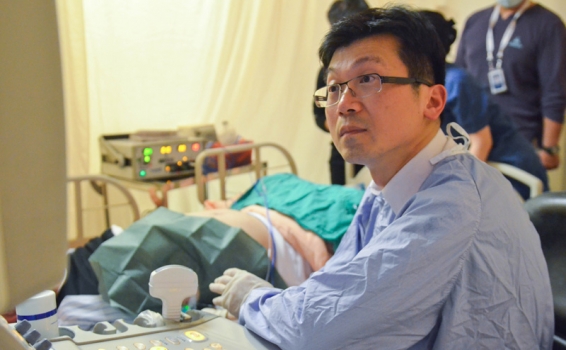
photo1: RFA can be performed in the ultrasound room without transferring to the operation room. The photo shows Director Chia-Chi Wang performing RFA.
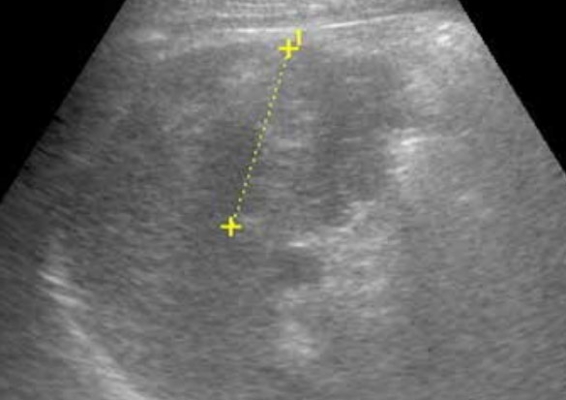
photo2: Before proceeding with cauterization, ultrasound is performed to identify and mark the tumor’s exact location to enhance treatment efficiency.
If the tumor is smaller than 3 cm in diameter and less than three categories, the patient can consider RFA . Since there currently two or multiple needle treatment, tumor under the size of 5 cm can be treated with a success rate of 90%. As the tumor increase in size, the success rate would decrease, and sometimes multiple treatment is required. In addition to primary liver cancer, RFA can also be used to treat few metastatic liver cancers or assist in chemical treatment to eliminate the remaining cancer cells. When the treatment completes, the front end of the needle can detect regional temperature, and the cancer cells are considered ablated once the temperature reached 60 degrees Celsius.
Dr. Chia-Chi Wang is the Director of Division of Gastroenterology and Hepatology, Taipei Tzu Chi Hospital. He is dedicated to researching a more effective and convenient therapy to reduce patients’ discomfort and restore health.
Tackle the Tumor without Surgeries
Radiofrequency ablation, which does not require a surgery, can be performed directly in the ultrasound room. Prior to the ablation, the patient must fast for six to eight hours, receive some painkillers and regional anesthesia, and under the guidance of ultrasound or CT scan, insert the needle through the skin and into the location of the liver tumor. The anesthetist would administer mild anesthesia for the patient to fall asleep. At this stage, the machine is turned on and cauterize the tumor cells. The time of cauterization varies due to tumor size, location and needle type. Once the treatment is over, the temperature of the cauterization is measured: if the temperature surpasses 60 degrees Celsius, then it has reached the standard. While the needle is in, the temperature would sustain at 80 degrees Celsius, which would reduce bleeding and the chance for tumor to spread. After the needle is removed, the patient must rest in bed, with sand bags pressurizing the wound for four hours to prevent bleeding.
Of course, any cancer treatment has its risks. RFA has a 1% chance of bleeding and infection, as well as some limitations. When the tumor is located neary colons, gallbladders or lungs, the heat may sometimes lead to colon perforation, pneumothorax, hemothorax or cholecystitis. A thorough evaluation is crucial to the injection of artificial ascites. If the tumor is located near large blood vessels or bile duct branches, the technique may cause hemorrhage or damage the bile duct and lead to stricture or jaundice.
Artificial Ascites: Greater Visibility and Insulation
Artificial ascites has two advantages: Visibility and insulation. First, water as a medium grants clearer vision of the tumor, which allows the insertion to be accurate. Liver cancer, for example, locates below the diaphragm, obstructed by air in the lungs, which prohibit ultrasound from identifying the tumor. Second, artificial ascites can act as an insulator during cauterization when the tumor is present near other vital organs to avoid any collateral damage.
Prior to injecting artificial ascites, a insertion point is selected at the abdominal region and is thoroughly sterilized. Take IV cannula, attach it to a syringe with 20 cc saline, and began the insertion slowly while pressing lightly on the syringe. If the saline can be injected into abdomen without any resistance, it means the needle has penetrated the abdominal wall and into the abdominal cavity. Now, insert 1 cm further so the catheter follows, then remove the hard needle and attach it to IV drip. If the drip flows smoothly and the patient is not in pain, the insertion is successful. In general, inject 1,000 to 2,000 cc saline to isolate the tumor from surrounding organs to about 5cm apart. Once the treatment is over, the ascites can be absorbed into the body after five to seven days. If the patient had previous surgical experiences, visceral adhesions may occur and reduce the success rate. Avoid injecting saline into the fascia, not only with it cause pain, but it would not have the intended effect.
During RFA, the patient may feel discomfort or even pain on the upper abdomen. Painkillers and mild sedatives used to be administered for pain relief, but more often than not the patient struggles during the treatment, causing the needle to relocate and reduces the treatment effectiveness. Our hospital enrolled the service of anesthetist to perform intravenous anesthesia, so the patient can sleep through the treatment without any burden of pain.
The winning formula to the treatment of liver cancer lies in early discovery and early treatment. The current goal is complete cure. In the case of severe liver cancer, the current trend is combination therapy: Combining embolization with cauterization, and even chemical, targeted drug and radiation therapies. It would also entail the collaboration among the departments of surgery, medicine, radiology, oncology and radiation oncology to bring tumors under control, improve the life quality of patients and extend their life span.
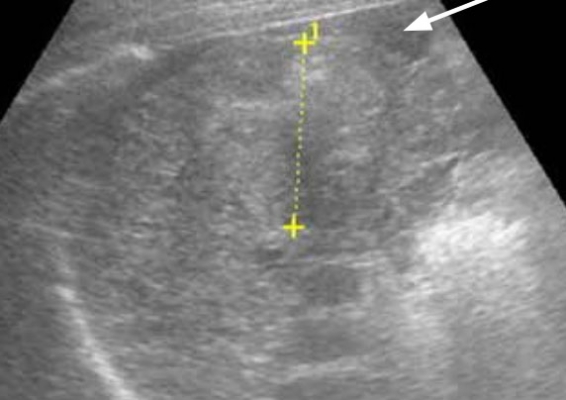
photo1: Prior to the injection of artificial ascites. The patient undergoes ultrasound to identify the location and size of liver tumor (indicated with a yellow marker, over 4 cm in diameter).
photo2: After the injection of artificial ascites. To perform cauterization on the tumor, the doctor injected artificial ascites between the tumor and colon (as shown by an arrow) to isolate colon and liver and act as a protective cushion.