A Documentary on Taipei Tzu Chi Hospital after Formosa Fun Coast Dust Explosion
On June 27, 2015, 8:40pm,
The worst burn accident in the history of Taiwan
took place at Formosa Fun Coast,
where the dust explosion injured 508 people.
Taipei Tzu Chi Hospital immediately
initiated mass casualty incident protocol,
mobilizing over 120 medical staff into rescue,
as 13 patients with burns ranging
from 40% to 90% body surface area arrived.
Medical and administrative staff collaborate seamlessly,
holding two interdisciplinary team meetings a day,
to update all changes on the patients’ conditions,
and to determine joint treatment plans.
Under the comprehensive care of
Tzu Chi medical team and volunteers,
two months went by,
and the patients were successfully discharged
one after another.
The road to rehabilitation is long,
and the love and care from the medical team
and volunteers will never cease...
/ Hsu Li-Hui
Around 9pm, June 27, all the news media ran the Formosa Fun Coast dust explosion on the newsflash. As the firefighters and paramedics rushed to the scene, hundreds of injured teenagers were wailing in pain. A party of fun and game turned into an inferno in a matter of only seconds.
Initiating Mass Casualty Incident Protocol
When Supt. Chao You-Chen received the news, he contacted the New Taipei City Fire Department at 9:30pm, notifying them that the Taipei Tzu Chi Hospital was ready to the patients. At 10:30pm, the New Taipei City Department of Health contacted the hospital that approximately twenty patients with 15% to 20% body surface area burned would arrive shortly. 10:47pm, the first burn patient, transported by the patient’s parents, arrived at the emergency room. After a brief assessment, the medical staff at the scene realized the severity of the burn was seriously understated: the total body surface area burn on this patient was at least 60%.
In preparation of the arriving burn patients, Yiang Giou-Teng, the director of ER, initiated the mass casualty incident protocol and corresponding ward bed arrangement. In addition to Supt. Chao, Vice Supt. Shyu Rong-Yuan, Vice Supt. Chang Heng-Chia, and Chief Secretary Chiao Li-Hua, over 120 medical professional, medical technologists, and administrative staff immediately returned to their post awaiting further instruction.
From 11:06pm to 12:33am, 12 patients transported by ambulance arrived at the hospital in succession. They were all very young, aging from 17 to 27, with 24% to 90% body surface area burn of 2nd and 3rd degree. Dir. Lu Chun-De, Dr. Wang Shu-Wei, and Dr. Lin Chung-Chiao from the plastic surgery, as well as doctors from ER, lead in stabilizing the patients’ conditions, while Night-shift Head Nurse Tsai Pi-Chueh coordinated the nurses to treat the wounds. “These patients were burnt all over. Aside from attending to the patient’s conditions, we needed four nurses cleaning the wound, draw blood, performing infusion, and administering IV drip, antibiotics, and tetanus shot simultaneously. If the patient suffers from inhalation burns, immediate intubation is required. In severe skin burns, if peripheral intravenous access cannot be achieved, central venous catheterization has to be performed while comforting patients as they scream in pain. Overall, we require a considerable amount of assistance,” said Dir. Yiang.
In terms of medical supply, antibiotics, burn creams, IV drips, and gauze were prepared by the pharmacy staff and property management team, providing sufficient logistic support to the frontline staff. To solace the anxiety of the family members, Supt. Chao awakened the volunteers from their dormitory to provide mental support for the distressed parents outside ER. Once the emergency treatment was completed, all the patients were transferred to ICU. At 2am, the department directors and social workers visited every single patient to understand their conditions and to discuss follow-ups.
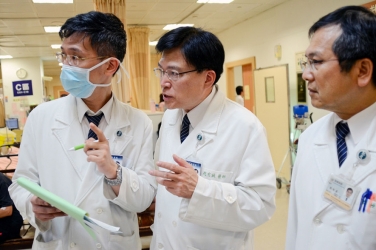
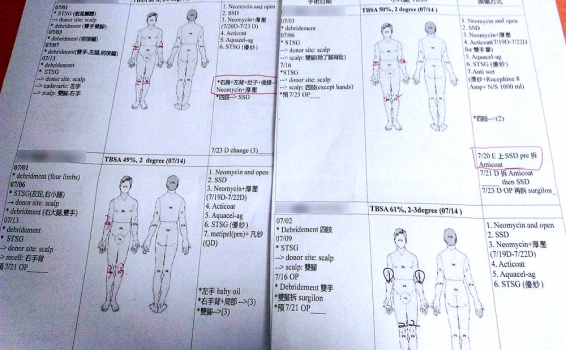
To ensure that everyone involved is updated on the patients’ conditions, Taipei Tzu Chi Hospital held a morning assembly every day at 8am, hosted by Supt. Chao, with hospital directors, director of surgical department, director of nursing department, social workers, volunteers, and staff from engineering affairs, general affairs, social services, medical affairs, information center, humanities, and public relations, discussing in detail on the medical and administrative operations. At 12pm, an expert meeting is hold with frontline medical staff, including staff from department of plastic surgery, infection, rehabilitation, psychosomatic medicine, nephrology, cardiology, thoracic, metabolism, gastrointestinal hepatobiliary, anesthesia, ICU, and head nurse, supervisor, nutritionist, psychologist, respiratory therapist, and pharmacist. Together they discuss the various perspective of every single patient’s physical and mental condition in scrutinizing details, and develop future treatment plans accordingly. Over 160 medical staff across multiple disciplines were devoted to the care of these 12 patients.
Non-stop Debridement and Skin Grafting for Plastic Surgeons
Taipei Tzu Chi Hospital admitted 13 burn patients immediately after the dust explosion incident. One more patient transferred in later from another hospital and two transferred out, which came to a total of 12 patients admitted. After 48 hours of emergency treatments to stabilize their conditions, these burn patients had to face their greatest challenge yet: infection. The Hospital set up a regulated burn area, managed by designated nursing staff, inside ICU where the burn patients were centralized, with positive pressure air conditioning to avoid infection. A video area was set up to allow the patients’ families to observe and communicate with the patients via video feed. All of these measures were taken to eliminate any chance of infection.
During the initial stage of treatment, several patients developed compartment syndrome, where the compartment begins to swell due to tissue inflammation and venous occlusion, the intercompartmental pressure continues to increase, causing impeded blood flow and eventually oxygen deprivation. The syndrome usually develops few hours or few days after the injury, which if left untreated, could result in muscle necrosis, secondary infection, nerve defects, gangrene, wound not healing, and even acute renal failure and death. The nurses closely observed the patients’ limbs to identify any swellings or numbness, and arrange fasciotomy when necessary to release the intercompartmental pressure and improve blood circulation.
July 1, Dir. Lu Chun-De, Dr. Wang Shu-Wei, and Dr. Lin Chung-Chiao from plastic surgery began wound debridement, where the dead skins are removed to avoid bacterial infection. Sometimes grafting and wound debridement were performed simultaneously to effectively reduce the burn surface. Three doctors, nurses, surgeon assistant, and anesthetist performed surgeries day and night, a surgical marathon that was a cruel test of their physical and mental endurance. Knowing that the team was understaffed, Dr. Yang Chih-Chao from Taichung Tzu Chi Hospital and Dr. Hsu Honda from Dalin Tzu Chi Hospital gave up their vacations to rotate with the exhausted staff, while Dr. Chuang Chun-Chi stayed for the entire month without taking a break in-between.
Improvised Ice Packs to Reduce Heat
When operating on patients with large surfaced burn, air conditioners in the operating room are switched off, and heat lamps on, to prevent the patients from hypothermia. The plastic surgeons have no options but to operate under a scorching 30 degrees Celsius temperature. Dir. Lu, who operated from 8am to 5pm, left the operating room with his entire garment soaked in sweat. Not one single drop of sweat can fall on the patient as it will risk infection.
The temperature in the operating room is usually set around 20 degrees Celsius where the bacteria are not too active, Dir. Lu explained, and in certain cardiac surgery, the temperature is lowered intentionally to reduce patient metabolism. When operating on burn patients, he added, the logic is reversed. When the patient’s body temperature drops below 36 degrees, the exposed body surface would lose moisture rapidly. To sustain a safe body temperature throughout the surgery, all air conditioners in the operating room are to be switched off, with additional heat lamps in place.
The empathetic nursing staff already made preparations before surgery to ensure that the surgeons could operate in their best conditions. They filled surgical gloves with water and iced it in a freezer, placed the ice gloves inside plastic bags, tied it under the surgeons’ surgical gowns to relief the heat.
In the middle of an operation, Dr. Lin received a bad news of his grandmother, who was suffering from colon obstruction and blood infection, was admitted into ICU after surgery. He was torn between his love for family and his obligation to the patient. “The saddest thing for the doctor is to be powerless when the family is ill,” Dr. Lin said. “I know very well who needs me the most at this moment.” Dr. Lin took the weekend off, rushed to the south to see his grandmother, and returned to his post the very next day.
Skin Grafting Machine Helps Accelerating Wound Healing
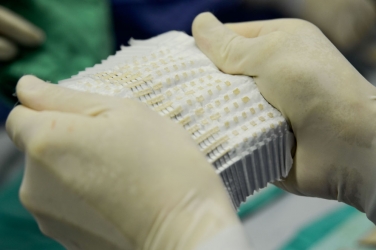
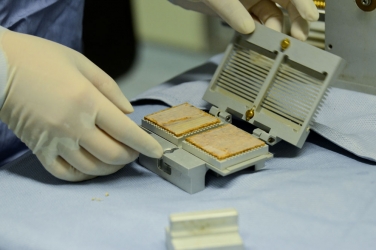
Autologous skin grafting, using patient’s own skin in grafting, can accelerate the wound healing in burn patients. The skins for grafting are usually harvested from thigh, hips or scalp. In the case of the Formosa Fun Coast survivors, majority of their lower limbs were burnt, which leaves the scalp as the sole supply of skin grafting. To minimize the number of surgeries and the pain it may cause, Dr. Lin arranged two skin grafting machines that can extend the skins, hence increase coverage, to nine times of its original size. Harvesting 4% of the skin from the scalp, for example, and extend that by ten folds, and you will have 36%, which is enough to cover both legs. “When we speak of 1% in body surface burn,” Dr. Lin explained, “we are referring to a burn surface equal to the size of a palm.”
Skin grafting machines are particularly useful for patients with large body surface burn, Dr. Wang added. Harvest a piece of skin, and the machine will cut it to small square pieces. Spray these pieces with bio-adhesives, paste it onto artificial dressing, and it can stretch nine times the original surface when unfolded. A week later, the grafted skins begin to receive blood supply from the patient, which then continues to grow, accelerate healing, and lower overall death rate.
Mobilizing the Entire Nursing Team
While these 12 patients resided in the burn area in ICU, each wound dressing or video conferencing requires a great deal of nursing staff. Each patient needs to dress the wound twice daily, each time an hour or longer, and since it is an extremely complicated and elaborative process, 8 nurses are required working seamlessly to complete it. In the case where the patient could not speak, a nurse has to accompany that patient, report the patient’s conditions in detail to the family members. Everyone gave everything to their assigned tasks, covering each other when needed, with no discrimination or complaints.
The head nurses of every department were responsible with the video conferencing. While the video conferences were being set up, the ICU nurses took the time to dress the wounds. Nurses from every department would, after finishing their own assignments, take shifts in ICU to cover for the ICU nurses. “Many nurses volunteered to take shifts in ICU. Someone of them just finished graveyard shifts, some of them were on vacation, and some were in the process of leaving the hospital,” said Wu Chiu-Feng, the director of Nursing.
A strong family support allowed ICU Head Nurse Kang Fang-Yu to concentrate fully on her job. “Why is mom not home? Can’t you come and do homework with me,” sometimes her child would ask. To that, she would clearly explain the tasks she was facing, “be good, there are many brothers and sisters in the hospital who needs my help.” Chen I-Ling, the head nurse of 11A, often brought her two children to the hospital, settle them down, and proceed straight to ICU. “There aren’t much I can do, so I want to do everything in my power to help out,” she said.
In response to the high demand of dressing staff, nurses who were experienced in intensive care or burn care teamed up into what was called a “dressing team”, with seven nurses a team, two teams in rotation (day shift and night shift). Before each dressing session, the team would hold a meeting, discussing the dressing methods and wound conditions of each individual patient. With each surgery, wound debridement, grafting, and dressing methods change accordingly. With the end of each shift, the members would again gather together to discuss wound conditions and dress techniques. Thanks to Nurse Wang ToJung, Chen Wen-Chun, Chen Huai-Yu, and Yu Wan-Ju who offered their support to Taipei Tzu Chi Hospital since June 28.
Supt. Chao was particularly grateful to senior nurse Wang To-Jung and Chen Wen-Chun. They hopped on the train when the news broke, went directly into the ICU to dress wounds after they arrived, worked 12 hours a day, taught the dressing teams methods and techniques, and established the initial dressing flow process and charts. “Thanks to their strictness, allowing our patients to receive the best care possible,” Supt. Chao said.
“The day shift usually begin at 8am and finish at 2pm,” 10B Head Nurse Chen Shu-Chuan recalled. “One day, a team working day shift just finished dressing the wounds at 3pm. Just as they were about to sit down and take a well-deserved rest, these nurses overheard a patient who accidentally wetted the wound. They stood up, went back in and redressed the wound.” During the first week, Nurse Chen felt as if her legs were no longer hers, aching and numbing all over. Human bodies are mysterious, though, she was used to it the second week.
Wound Dressing Manual for Nurses and Patients
From preparing medicine, undressing, unpacking, clean, dressing, apply crepe bandage, apply gauze, change bed sheet, to cleaning the patient’s body, every single procedure is critical. Eight nurses must each complete their assigned tasks. Injuries on different parts of the body must be dressed differently. “When dressing, everyone is responsible for a certain region where no one else can touch,” said Heart Lotus Ward Head Nurse Chen MeiHui. The strict rule is in place to avoid the risk of infection.
To shorten dressing time and minimizing patient pain, the nursing team developed their own dressing manual, documenting in detail the conditions, burned areas, and dressing procedures of individual patient. It is a perfect example of the mindfulness and patience of our nurses.
Dressing the wounds of a burn patient can be a delicate undertaking. Even the slightest movement when dressing can evoke excruciating pain. “Every time we undress the wound, a slightest touch to the limb and the patient trembles in pain. We pause whenever they wail. The degree of pain is simply beyond our imagination. Patients who suffer from lung burn lacked the strength to cough on their own, we had to tap their back to assist the coughing. Every time, they would beg us to stop, and that is when our tears fall,” Lin Yu-Ting, senior nurse at ICU, said. Despite the pain, there were several patients who would endure and say, “thank you for everything!”
Consolation from nurses is an excellent alternative to anesthesia. When dressing wound, Head Nurse Kang FangYu would comfort the patients, “I am going to clean the wound! Count with me, one, two, three! I am going clean again now,” distracting the patients from pain by keeping them engaged.
During the video session on the first day, Palliative Care Head Nurse Chen MeiHui had just completed dressing a 20 year old girl and accompanied her in the video chat with her family. The girl trembled in pain throughout the entire session. “Dad, do you still love me? I should’ve listened to you and not attend the party. Please, don’t be sad, I am sorry,” she said. “As soon as you recover, I will take you anywhere you want to go,” her father said, visibly holding his tears in. The dialogue repeated again and again, between parent and child in their first conversation since the incident.
Anesthetists Tried Keeping Pain Away
Pain, for burn patients, is a constant, haunting nightmare, which makes anesthesia a must in the treatment and recovery of burn patient. As the dust explosion survivors started to arrive at the Hospital, the anesthetists immediately reported to ER, performing central venous catheterization to maintain patient vital signs. They would be needed again in debridement and skin grafting once the patients stabilizes to administer general anesthesia.
One day after the incident, the Department of Anesthesiology organized a pain treatment team, responsible for pain relief, anesthesia, and acute and chronic pain management. They fully utilized the essence of empirical medicine, collecting and reviewing literature to discuss with experts of all fields involved.
Since the burn patients had to endure the skin-ripping pain twice a day, the medical staff would administer morphine prior to wound dressing. The amount, though, must be precise to relieve pain without placing them in deep sleep, risking the chance of never waking up.
During the initial phase (acute stage) of the treatment, morphine remains the primary pain reliever, said Kao MingChang, Director of Pain Clinic. Some hospitals introduced patient-controlled anesthesia (PCA), where the medication and dosage is regulated by an anesthetist depending on patients conditions, allowing patients to self-administer morphine for fast pain relief. Because burn patients admitted to Taipei Tzu Chi Hospital suffered large body surface burn including the limbs, which prohibited them from controlling their fingers, administration of intravenous morphine was decided as the primary pain relief method, in conjunction with non-morphine, neuralgia or chronic pain medication, to reduce drug dependence and prevent chronic pain.
“I have been pondering, is morphine the only solution to the acute pain of these children,” Dir. Kao wondered. In the numerous discussions Dir. Kao had with experts, they all agreed on the benefit of administering large dosage of morphine to the patient, the thought of injecting these young people with schedule 1 substance on daily basis continued to keep him up at night. Intravenous injection is a fast and effective pain reliever, but fast pain relief can lead to dependency and eventually addiction. The concern haunted Dir. Kao until the administration of intravenous morphine discontinued.
Mr. Huang, who was particularly sensitive to pain, demanded the presence of pain physician when dressing. “When I see Dir. Kao, I see him as a guardian angel. He is like pain killer, whenever he is around, the pain is not as unbearable,” Mr. Huang claimed. “Sometimes the patient is relieved simply by having us around. Our presence alone offers a psychological consolation. The profession and obligation of anesthetists and pain physicians is to help patients in identifying the most appropriate pain relieved, so they won’t be scarred with a horrible memory throughout the treatment,” Dir. Kao shared.
Peripheral Vascular Team Saving Injured Limbs
Chang, age 18, suffering from severe burn in her lower limbs, had trouble sleeping due to lower limb pain since hospitalized. The pain in her lower right limb persisted despite pain killers, Supt. Chao pointed out. He asked the director of Cardiovascular and Peripheral Vascular Center Dr. Huang Hsuan-Li to arrange a catheter examination, and the result indicated a 13cm blood clot lodged somewhere between her iliac artery and common femoral artery.
Dir. Huang frowned when he first saw Chang’s result, the severity of the injury was worse than expected. “Blood flow to her right leg is restricted, a surgeon may recommend amputation. We used vascular ultrasonography when dressing her wound to assess the blood flow, discovering that the blockage happened somewhere in the abdominal blood vessels, restricting blood flows from the heart to the right leg. It has a great impact on wound dressing and debridement, no blood flow means the risk of necrosis,” Dir. Huang explained. If the blood vessels are not cleared in time, it could lead to amputation above the knee.
The peripheral vascular team used cardiac catheterization to clear Chang’s abdominal artery, using guide wire and thrombectomy catheter to remove the 13cm blood clot, and opened up the restricted arteries with balloon angioplasty, placed a new type of blood stent to ensure unobstructed blood flow from the heart to the feet. Chang could finally have a good night sleep without the persistent, disrupting pain. Chang was Dir. Huang youngest patient, as well as his first burn patient, he did all he could for Chang despite the harsh challenges.
Although the artery in Chang’s right leg opened up nicely days after the operation, many blood capillaries around the region remained clogged. A right leg amputation below the knee was performed to save her life. Considering how hard it must for Chang to accept, a hospital director contacted Chou Yaching, a girl who had her left lower limb amputated last year, to share her experience and challenges with Chang and her family, letting them know that an amputee can still lead a splendid life.
Chang almost broke down when Supt. Chao broke the news to her about the amputation. Her mother, too, was saddened by the news. The encouragement from Chief Secretary Chiao, Social Worker Yang, and her classmates eventually calmed Chang’s heart. After the amputation, Supt. Chao and Chief Secretary Chiao visited Chang often in her ward, Chang’s classmates chat with her via internet, and Chou took her weekends to accompany Chang in her recovery. Two months later, Chang’s condition finally stabilized and was transferred to general ward. Her mood, too, had stabilized. She was ready to face the long rehabilitation ahead.
Out of the 12 burn patients admitted to Taipei Tzu Chi Hospital, one unfortunately passed away, the rest were transferred out of ICU into general ward, and few successfully discharged. The medical team used everything they had to save the lives of these young patients and console their fear and anxiety. Three month long treatment exhausted and fatigued countless hospital staff, some had fallen ill, but the treatment and accompaniment continued. The complete and unwavering trust from the patients and their family was the driving force that supported Taipei Tzu Chi Hospital team in their mission to save lives.